Subscribe to our newsletter
We’ve all been sold the dream of seamless EHR integration, yet most of us are living in a reality of digital duct tape and constant workarounds. The promise of unified patient care remains stubbornly out of reach, blocked by a tangle of legacy interfaces, mismatched data, and workflows that frustrate clinicians. This isn’t just an IT problem; it’s a direct threat to operational efficiency and patient safety. This article provides a no-nonsense playbook for hospital leaders. We will diagnose the five most chronic EHR integration challenges, quantify their impact in dollars and risk, and lay out an actionable solution combining modern middleware, disciplined processes, and the right people. It’s time to stop patching the old and start building the future.
The Five Wounds of a Broken Integration Strategy
I once spent an entire weekend in a hospital data center with a box of stale donuts, trying to figure out why our new smart infusion pumps were sending garbage data to the Epic® EHR. The vendor blamed us; we blamed them. The problem? A single, undocumented custom segment in a 20-year-old HL7 admission feed was corrupting the patient identifier downstream. The pumps couldn’t match the patient. The nurses couldn’t trust the automation. Sound familiar?
That one weekend was a symptom of a deeper disease. These are the five chronic obstacles we see crippling health systems today.
1. The Tyranny of Brittle, Point-to-Point Interfaces
This is the classic “spaghetti diagram” problem. Every new system—labs, radiology, billing—gets its own unique, hand-coded connection to the EHR. This web of legacy interfaces is fragile and expensive. When the EHR is upgraded, dozens of interfaces break simultaneously.
- The Impact: The average cost to build and maintain a single, complex interface can exceed $100,000 over five years. Multiply that by the hundreds of interfaces in a typical health system, and you’re looking at a multi-million-dollar hidden tax on your IT budget.
2. The “Semantic Abyss” of Data Mapping
Your Cerner® system calls it “Systolic BP.” The newly acquired clinic’s Allscripts® system calls it “SBP.” The reference lab calls it “Blood Pressure-Systolic.” They all mean the same thing, but the systems don’t know that. This is the data mapping nightmare. Teams spend countless hours manually translating data fields, a process that is both mind-numbingly tedious and dangerously prone to error.
- The Impact: A single mapping error—mistaking milligrams for micrograms—is a “never event” waiting to happen. The risk is incalculable.
3. The Workflow Disconnect
Technology that doesn’t fit the clinician workflow gets ignored or worked around. We install a state-of-the-art patient monitoring system, but if viewing its data requires a nurse to log into a separate computer, they’ll just go back to writing it on the whiteboard. The integration “works” technically, but fails operationally.
- The Impact: A study from AORN found that interface and system failures can add an average of 45 minutes to surgical case turnover time.1 That’s lost revenue, frustrated surgeons, and delayed patient care, all because the tech didn’t align with the real-world process.
4. The “Accidental” Architecture
Most health systems didn’t design their integration strategy; it just… happened. One department bought a system, another bought a different one. The IT team was told to “make it work.” This lack of a central plan leads to redundant tools, conflicting standards, and zero economies of scale. It’s an architecture built by chance, not by choice.
- The Impact: This chaos forces you to solve the same problem repeatedly. We found one health system that had purchased three different integration engines for three different departments. They were paying three times for the same capability.
5. The Widening Talent Chasm
The number of engineers who are fluent in both ancient HL7 v2 and modern FHIR APIs is vanishingly small. And they are incredibly expensive. Trying to staff an in-house team to manage a complex, hybrid integration environment is a losing battle against the tech industry’s deep pockets.
- The Impact: Key-person dependency becomes a major operational risk. When the one person who understands the lab interface goes on vacation (or quits), progress grinds to a halt.
The Playbook: A Modern Approach to EHR Integration
Fixing these problems requires more than a new piece of software. It demands a deliberate strategy built on three pillars: the right tools, disciplined processes, and empowered people.
The Tool: A Modern Middleware Platform
You can’t build a skyscraper on a foundation of sand. You need to replace the spaghetti mess of point-to-point connections with a modern integration layer. This isn’t just one piece of software, but a stack of capabilities.
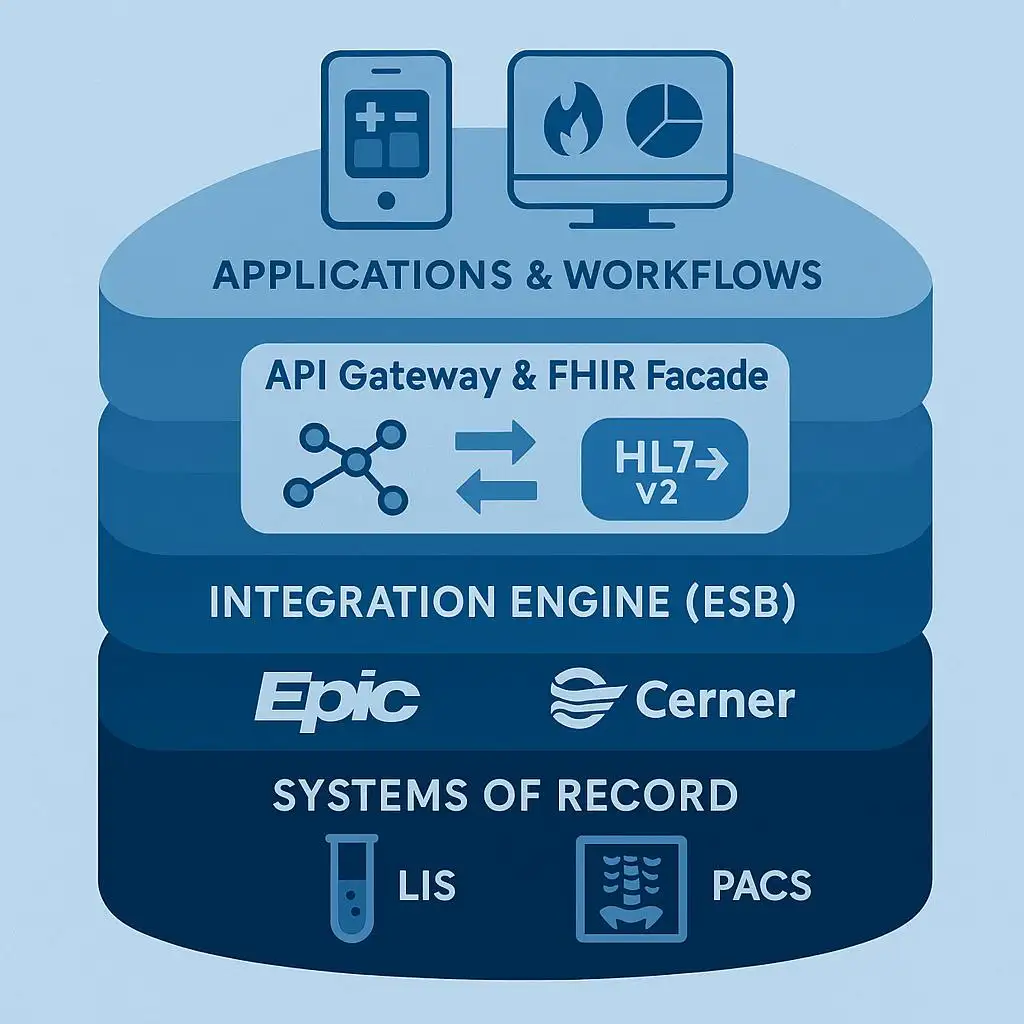
This stack typically includes:
- An Integration Engine/ESB: The workhorse that handles legacy HL7 and other data formats. It centralizes the routing and transformation of data.
- An API Gateway: The secure front door for all modern data access. It manages, secures, and logs every API call.
- A FHIR Façade: A critical component that translates data from legacy formats (like HL7 v2) into standardized FHIR resources on the fly. This lets you expose your old systems via a modern API without having to rip and replace them.
A mature middleware platform like this, whether from a single vendor or assembled from best-of-breed components, gives you a single point of control and visibility. For a more tailored solution, a partner like Logicon can help implement these tools with pre-built accelerators to speed up the process.
The Process: Discipline and Measurement
A great tool with bad processes just helps you make messes faster. The key is to establish clear governance and metrics for success.
- Establish an Integration CoE: Create a cross-functional Center of Excellence with members from IT, clinical operations, and finance. This team owns the integration roadmap and is the single point of contact for all new interface requests.
- Standardize Everything: Define your canonical data models. There will be one, and only one, way to represent a patient’s blood pressure. All systems will map to this central standard.
- Set Aggressive KPIs: You can’t improve what you don’t measure. Target clear performance goals. We aim for:
- Time-to-first-interface < 90 days for a new data feed.
- Critical interface downtime < 15 minutes per quarter.
The People: Empowering a Central Team
Your CoE is responsible for strategy and governance, not for writing every line of code. Their job is to enable the rest of the organization. They provide a “paved road”—a set of standard tools, APIs, and best practices—that makes it easy for application teams and even third-party vendors to connect to your ecosystem securely. This frees up your best engineers to work on high-value innovation instead of low-value plumbing.
Stories from the Field
The M&A Accelerator
A 400-bed regional health system was drowning after acquiring two smaller hospitals. They had a backlog of 75 critical interfaces needed to connect the new facilities’ EHRs and billing systems. Their old point-to-point method would have taken two years. Instead, they invested in a commercial middleware platform. By creating a standard set of FHIR APIs for their core data (Patient, Encounter, Orders), they were able to connect the first hospital in five months and the second in four. They cleared their backlog 60% faster than projected.
Solving the Workflow Disconnect
An academic medical center wanted to give its intensivists a real-time, unified view of patient data from the EHR, ventilator, and IV pumps on a single mobile dashboard. The data existed, but in three different silos. Using their integration platform’s FHIR facade, they exposed data from all three systems through a single, secure API. A small innovation team then built a SMART on FHIR app that consumed this API. The result: a dashboard that went from concept to pilot in 12 weeks, giving clinicians the unified view they’d been asking for for years.
Your 5-Minute Integration Self-Audit
Ask your team these five questions. The answers will tell you how healthy your EHR integration strategy is.
- The Bus Test: If our lead interface developer won the lottery tomorrow, would any of our critical systems go down within a week?
- The New App Test: How long would it take, in weeks, to provide a new application with secure, read-only access to a patient’s active medication list?
- The Upgrade Test: When we last upgraded our core EHR, how many interfaces broke, and how many person-hours did it take to fix them?
- The CFO Test: Can we quantify the total annual cost of our integration—including licenses, maintenance, and developer salaries?
- The Nurse Test: Can a floor nurse name a single integration project from the last year that measurably made their job easier?
If the answers make you uncomfortable, it’s time for a new plan.
Let’s Build Your Roadmap
Overcoming these challenges is a journey, not a single project. But you don’t have to do it alone. A clear, strategic roadmap is the first step toward leaving the chaos of accidental architecture behind.
Book a complimentary, no-obligation integration roadmap session with a Logicon expert today.