Subscribe to our newsletter
Disclaimer: This article is for informational purposes and does not constitute financial or medical advice.
In healthcare, the pressure is relentless. Do more with less. Boost throughput. Cut costs, but improve quality. For operations leaders and innovators, this is the daily tightrope walk. For years, we’ve been told that data is the answer, yet most of us are still drowning in it, using spreadsheets and historical reports to make mission-critical decisions. But what if you could know with 85% certainty how many patients will arrive in your ED next Tuesday? Or which MRI machine is likely to fail next month? This isn’t science fiction. It’s the reality of advanced healthcare operations analytics. This article explores the journey from basic reporting to true, AI-driven prescriptive guidance. We’ll break down three high-impact use cases—predictive staffing, patient-flow optimization, and predictive maintenance—and show how leading health systems are using them to transform efficiency and patient care.
More Than a Rear-View Mirror: The Analytics Maturity Curve
I remember sitting in an operations meeting years ago, looking at a stack of reports that were already two weeks old. We were analyzing last month’s overtime costs, trying to understand why we were so over budget. We were steering the ship by looking at its wake. That’s descriptive analytics. It tells you what happened. It’s essential, but it’s fundamentally reactive.
To truly transform operations, we have to move up the analytics maturity curve. This is a journey from hindsight to foresight. It’s about evolving your data from a historical record into a predictive, decision-making engine. Most health systems use descriptive and diagnostic analytics today. The fundamental transformation, however, happens when you climb higher.
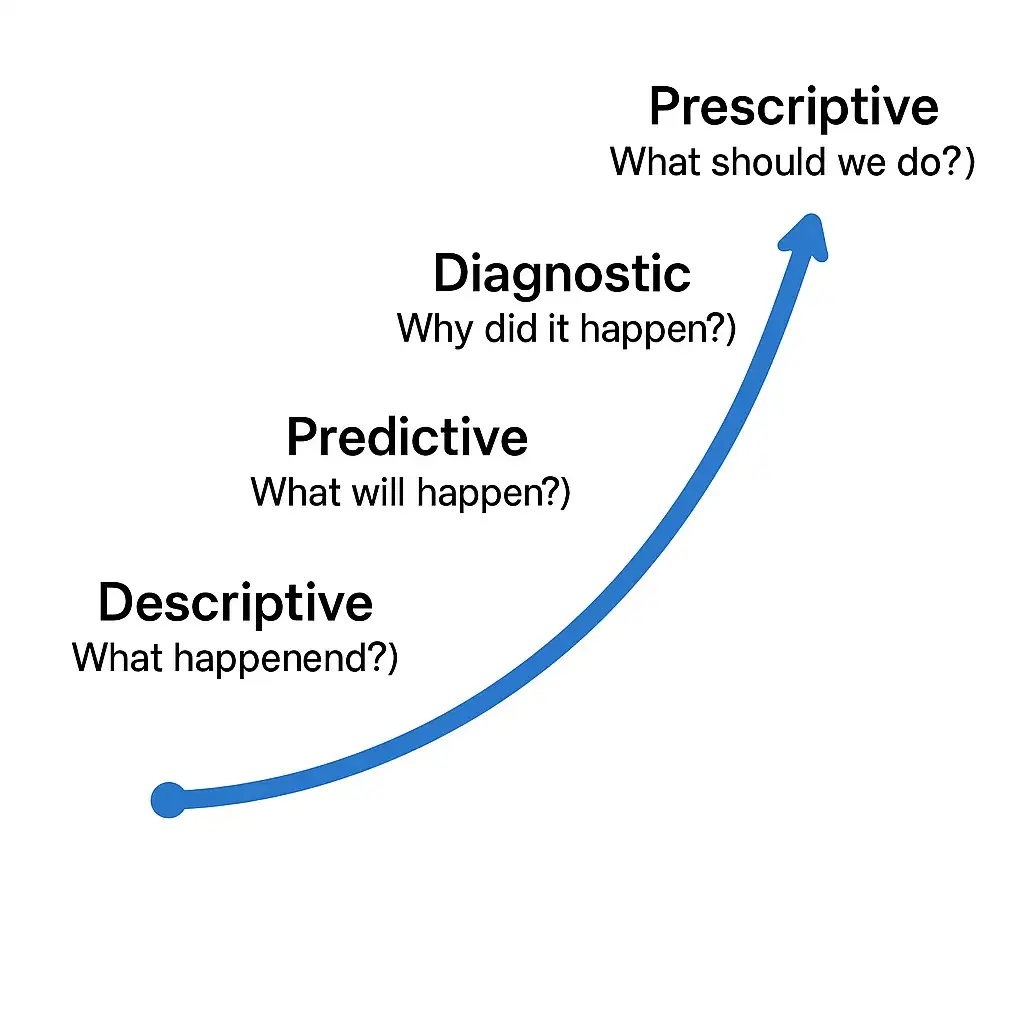
Here’s a quick breakdown of the four stages:
- Descriptive Analytics: What happened? This is your basic dashboard showing historical data, like last quarter’s patient volumes or average length of stay (LOS).
- Diagnostic Analytics: Why did it happen? This layer drills down to find root causes. For example, it connects a spike in readmissions to a specific care pathway or staffing level.
- Predictive Analytics: What will happen? This is where it gets exciting. Using machine learning models, you can forecast future events, such as patient demand or equipment failure.
- Prescriptive Analytics: What should we do about it? The highest level of maturity. Here, the system doesn’t just predict an event; it recommends an optimal response, like automatically adjusting nurse schedules or ordering a specific part for an MRI machine.
For leaders like Ivy and Omar, moving up this curve is the single most powerful way to drive efficiency. Let’s look at three practical examples.
Use Case 1: Beyond the Spreadsheet with Predictive Staffing
The old way of staffing is a nightmare. It’s a constant battle between budget and burnout. Overstaff and you blow your labor budget on idle hands. Understaff and you burn out your best nurses, compromise patient safety, and pay a fortune in overtime.
The Solution: Predictive staffing models use AI to create hyper-accurate demand forecasts. These models analyze years of historical admissions data, but they also layer in external factors: local school schedules, community events, flu season trends, and even weather forecasts. Instead of relying on a manager’s gut feeling, you get a data-driven prediction of patient load by unit, by shift.
The Proof: Health systems are already seeing incredible results. Hartford HealthCare, for instance, used its AI-driven optimization system to reduce overtime expenses by 15% and increase staff utilization by 20%. This isn’t just a financial win; it’s a massive win for your team. When staffing aligns with actual demand, clinicians feel supported, not swamped. From a clinical standpoint, appropriate nurse-to-patient ratios are directly linked to better outcomes and lower mortality rates. It’s one of the clearest examples of how operational analytics directly impacts patient safety.
Use Case 2: Solving the Gridlock with Patient-Flow Optimization
Every operations leader knows the feeling of gridlock. The ED is on divert because there are no inpatient beds. Discharges are delayed waiting for a final sign-off. Patients are waiting hours for a clean room. It’s a complex, system-wide ballet where one missed cue can bring everything to a standstill.
The Solution: AI-powered patient-flow optimization acts as the hospital’s air traffic control system. It provides a real-time, system-wide view of capacity and bottlenecks. More importantly, it uses predictive models to see traffic jams before they happen. The system can flag a patient who is an ideal candidate for early discharge planning, predict when an ICU bed will become available, and automatically prioritize housekeeping requests for rooms in high-demand units.
The Proof: The impact on length of stay (LOS) is dramatic. Memorial Hospital at Gulfport implemented a data-driven approach that cut its average LOS by nearly half a day (0.47), leading to $2 million in cost savings. I’ve seen firsthand how crucial integration is to making this work. You can have the most innovative AI model in the world, but if it can’t get real-time ADT data from the EHR, bed status from the environmental services app, and transport requests from the logistics system, it’s useless. A robust interoperability backbone is the prerequisite for advanced patient flow analytics.
Use Case 3: From Reactive to Proactive with ML Maintenance
Few things cause more chaos than a critical piece of equipment going down. When an MRI or CT scanner fails unexpectedly, the fallout is immediate: canceled appointments, lost revenue, frustrated physicians, and delayed diagnoses. The cost of unplanned downtime for a single MRI can be staggering, with some estimates putting the lost revenue between $60,000 and $120,000 for an outage of 30 to 60 hours per year.
The Solution: Predictive maintenance, sometimes called ML maintenance, embeds IoT sensors in your critical equipment to monitor operational data—vibration, temperature, error codes, and image quality metrics. A machine learning model analyzes this stream of data to detect subtle anomalies that signal an impending failure. Instead of an emergency call at 2 AM about a broken scanner, you get an alert that says, “The gradient amplifier on MRI 2 is showing a 90% probability of failure within the next 7-10 days.”
The Proof: This shifts your entire maintenance strategy from reactive to proactive. You can schedule repairs during off-hours, order parts without paying for rush shipping, and avoid almost all unplanned downtime. The ROI is clear and immediate. Beyond the direct cost savings, the clinical benefit is ensuring that a patient’s care journey is never delayed because of a broken machine. It builds trust with referring physicians and ensures your multi-million dollar assets are generating revenue, not collecting dust.
Early ROI Benchmarks: What to Expect
While results will vary, these use cases have a proven track record of delivering tangible returns. This is the kind of data that gets a CFO’s attention.
| Use Case | Key Metric Improved | Conservative Benchmark | Illustrative Annual Savings (for a 350-bed hospital) |
| Predictive Staffing | Overtime Cost Reduction | 15% | $750,000 |
| Patient-Flow Optimization | Length of Stay (LOS) Reduction | 0.4 days | $1,800,000 |
| Predictive Maintenance | Unplanned Downtime Reduction (MRI) | 50% | $150,000 per scanner |
Disclaimer: All financial figures are illustrative and for estimation purposes only. Actual ROI will vary based on organizational scale, baseline performance, and implementation quality.
The Future is Now
Moving up the analytics maturity curve isn’t about chasing shiny objects. It’s about fundamentally re-engineering how your hospital operates. By shifting from reactive reporting to proactive, AI-driven guidance, you can solve some of the most persistent challenges in healthcare: staff burnout, operational bottlenecks, and wasted resources.The technology in healthcare operations and analytics is ready. The question for every hospital leader is: Are you?