Subscribe to our newsletter
The rapid adoption of telehealth has created a new, urgent challenge: fragmentation. When virtual care platforms operate in silos, disconnected from the core Electronic Health Record (EHR) and operational systems, they can lead to inefficiencies and poor patient outcomes. The result is crippling inefficiency, frustrated clinicians, and a disjointed patient experience. A strategic approach to telehealth integration is no longer optional. It’s the critical next step for any health system aiming to deliver genuine hybrid care. This guide provides a blueprint for executives, outlining the architectural principles, implementation playbook, and measurable ROI of creating a unified care ecosystem. By connecting disparate systems, organizations can slash administrative overhead. Improve provider productivity and build a scalable foundation for the future of healthcare delivery.
The Integration Imperative: From Fragmented Tactics to a Unified Strategy
The promise of telehealth was a seamless “digital front door.” For many, the reality is a maze of disconnected hallways. Clinicians toggle between screens, manually re-entering patient data. Schedulers wrestle with multiple calendars, leading to double-bookings and patient confusion. From an operational standpoint, it’s a recipe for inefficiency and staff burnout. For leadership, it’s a strategic blind spot.
This isn’t a niche issue. Recent studies show that a staggering 78% of healthcare executives cite the lack of integration between their telehealth platforms and EHRs as a significant challenge. This disconnect directly undermines the very goals telehealth was meant to achieve.
For a Operations Director, this fragmentation manifests as daily friction:
- Increased Staff Workload: Nurses and administrative staff spend hours transcribing virtual visit notes, uploading documents, and reconciling schedules, pulling them away from patient-facing activities.
- Compromised Patient Flow: A lack of real-time scheduling updates between in-person and virtual appointments leads to higher no-show rates and underutilized clinical resources.
- Inconsistent Care Quality: If a provider in a virtual visit can’t easily access a patient’s full history from the EHR, they are working with incomplete information, increasing clinical risk.
For a CIO, the challenges are architectural and strategic:
- Data Silos: Patient data generated during virtual visits remains trapped in the telehealth platform, invisible to enterprise analytics, population health initiatives, and quality reporting.
- Security & Governance Gaps: Managing patient identity, access control, and data security across multiple, non-integrated systems creates significant compliance vulnerabilities.
- Inability to Scale: Without a unified data backbone, launching new virtual service lines or expanding hybrid care models becomes an expensive, time-consuming custom project every time.
The path forward lies in treating telehealth integration not as a one-off IT project, but as a core tenet of your enterprise architecture.
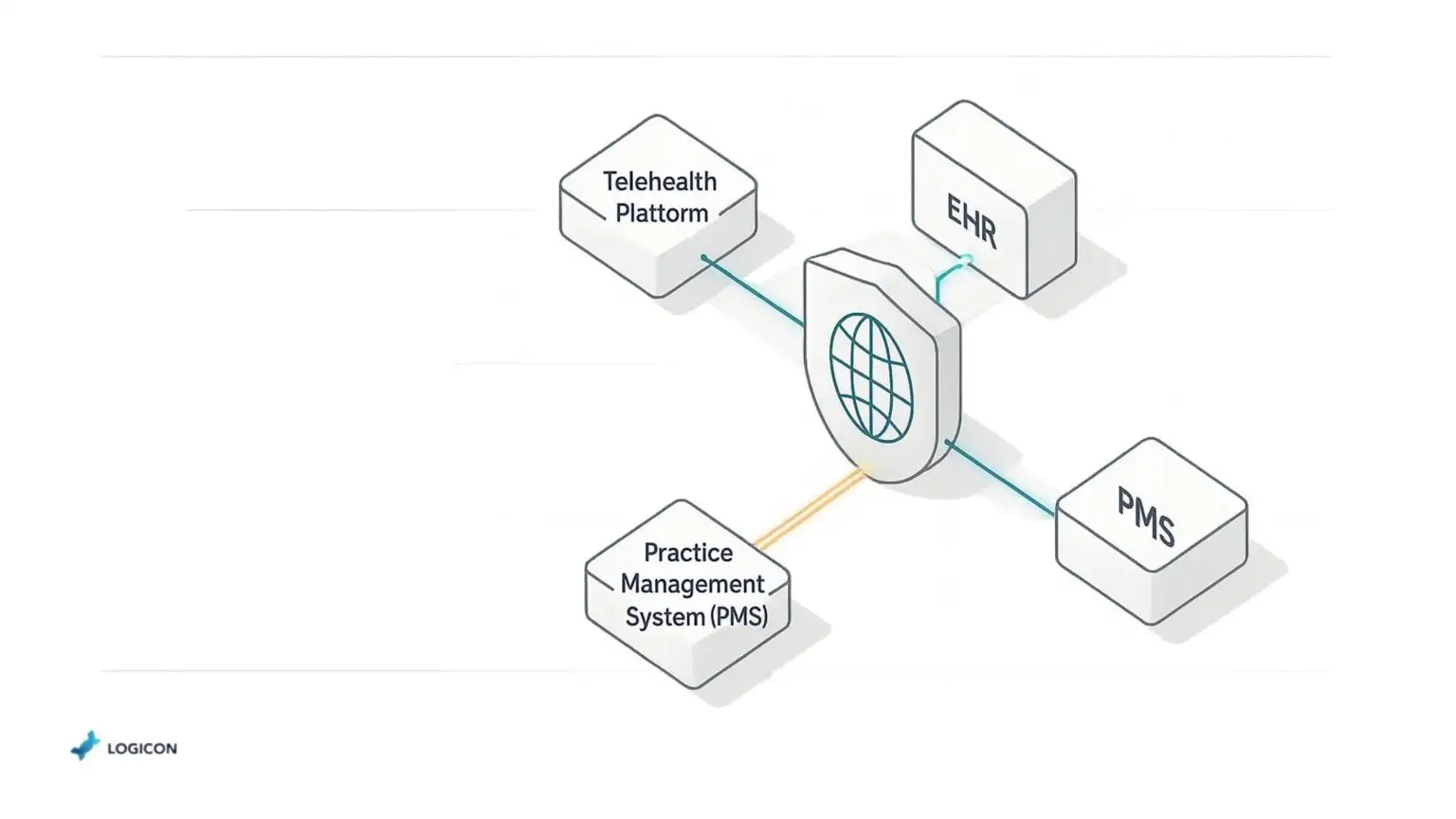
Architecting Seamless Virtual + In-Person Care
A robustly integrated telehealth ecosystem isn’t magic; it’s the result of deliberate architectural decisions. The goal is to create a secure, bidirectional flow of information that makes the boundary between a virtual visit and an in-person appointment invisible to both patient and provider.
Data Exchange Standards: The Lingua Franca of Health Data
Effective integration starts with a common language.
- HL7 (Health Level Seven): For decades, HL7 v2 and v3 have been the workhorses of health data exchange, primarily for pushing information between established systems like the EHR, lab systems, and billing engines. They are essential for connecting with legacy infrastructure.
- FHIR (Fast Healthcare Interoperability Resources): The modern standard, FHIR (pronounced “fire”), is a game-changer. It’s an API-based approach that treats data as discrete, web-friendly resources (like a single patient profile, an appointment, or an observation). This makes it far more flexible and lightweight than HL7, perfect for mobile apps and modern cloud platforms.
- SMART on FHIR: This is a security and app-launch protocol that sits on top of FHIR. It allows third-party applications (like a specialized telehealth solution) to plug directly into an EHR or patient portal, creating a seamless user experience without complex custom coding.
Identity & Access Management: One Patient, One Chart, One Login
Data integrity and security hinge on knowing who is accessing what information.
- Single Sign-On (SSO): For clinicians, SSO is a must. It allows a provider to log in once and gain secure access to the EHR, the telehealth platform, and other clinical tools without juggling multiple passwords. This simple step saves time and reduces login-related IT support tickets, a direct win for operational efficiency.
- Robust Patient Matching: When a patient registers on a telehealth app, the system must be able to accurately and automatically match them to their existing record in the EHR. Poor matching creates dangerous duplicate records and fragmented patient histories. A sophisticated integration strategy employs master patient index (MPI) algorithms to ensure a single, authoritative source of truth for every patient.
Real-Time Data Synchronization: The End of the Nightly Batch
Yesterday’s data is a liability in today’s fast-paced clinical environment.
- Event-Driven Architecture: Modern integration platforms operate in real-time. When a patient books a virtual appointment, an “event” is triggered that instantly updates the EHR schedule. When a provider signs a virtual visit note, it’s immediately available in the patient’s chart.
- vs. Batch Processing: The old method of running “nightly batches” to sync data is no longer adequate. It creates a 12- to 24-hour lag, meaning a primary care physician might not see the notes from an urgent virtual care visit until the next day. This delay impacts care coordination and frustrates providers.
Legacy Compatibility Tactics: Bridging the Old and the New
No health system is a blank slate. A successful integration strategy must embrace and extend the life of valuable legacy systems.
- Middleware: This is the technological “glue” that connects systems that weren’t designed to talk to each other.
- Enterprise Service Bus (ESB) vs. API Gateway: An ESB is a traditional, centralized middleware hub that can connect many systems, but can also become a bottleneck. A more modern approach uses an API Gateway, which acts as a secure front door for all data requests. This method, often part of a microservices architecture, is more flexible, scalable, and easier to manage, allowing partners like Logicon to build resilient, future-proof connections.
Implementation Playbook: A Disciplined Approach to Rollout
A successful telehealth integration project balances speed with stability. Rushing a deployment can disrupt clinical operations, while moving too slowly delays the realization of benefits.
Phased Rollout vs. “Big Bang”
| Approach | Pros | Cons | Best For |
| Phased Rollout | Lower risk, allows for learning and iteration, less disruption to operations, faster time-to-value for initial pilot groups. | A longer overall project timeline requires careful management of parallel systems during transition. | Large, complex health systems with diverse service lines and low risk tolerance. |
| “Big Bang” | All users move to the new system at once, resulting in a shorter project timeline and eliminating the need for parallel systems. | Extremely high risk, potential for significant operational disruption, and any failure has system-wide impact. | Smaller, less complex organizations with a high tolerance for risk and a critical need for rapid change. |
7-Step Agile Rollout Checklist
For most enterprise health systems, a phased, agile approach is superior.
- Discovery & Auditing: Map all existing workflows, data sources, and systems involved. Identify key stakeholders from clinical, operational, and IT departments.
- Define KPIs & Success Metrics: Establish the baseline for metrics like no-show rates, provider documentation time, and A/R days.
- Architect the Solution: Design the integration flow based on FHIR APIs, legacy needs, and security requirements. This is where an experienced integration partner is invaluable.
- Develop & Configure: Build and configure the interfaces, connectors, and data transformation rules within the integration engine.
- Automated Testing & DevOps: Rigorously test every workflow. Employ DevOps principles like Continuous Integration/Continuous Deployment (CI/CD) to automate testing and deployments. Ensuring that updates can be pushed safely and reliably without system downtime. This appeals directly to a CIO’s need for stable, well-governed IT operations.
- Pilot Program: Launch the integrated solution with a single, enthusiastic service line or clinic. Gather feedback, resolve issues, and validate the ROI.
- Scale & Optimize: Based on the successful pilot, incrementally roll out the solution across the organization. Continuously monitoring KPIs and optimizing workflows.
The ROI & KPI Dashboard: Measuring What Matters
A strategic telehealth integration initiative delivers clear, quantifiable returns that resonate from the boardroom to the clinic floor.
- Dramatically Reduced Patient No-Shows: By integrating scheduling systems for automated, real-time reminders and confirmations, health systems see no-show rates fall by an average of 67%.
- Increased Provider Productivity: Eliminating the “swivel chair” interface and manual data entry gives clinicians back valuable time. Seamless documentation workflows can boost provider productivity by an average of 12%.
- Lowered Administrative Overhead: Automating tasks like eligibility checks, prior authorizations, and results. Routing can reduce associated administrative costs by approximately 18%.
- Accelerated Revenue Cycles: When virtual visit coding and documentation are integrated directly into the billing system. Charge capture becomes faster and more accurate, reducing Accounts Receivable (A/R) days by an average of 9%.
Calculating Your Payback Period:
While every implementation is unique, you can estimate the payback period with a simple formula:
Payback Period (in months) = (Total Initial Implementation Cost) / (Combined Monthly Cost Savings + New Revenue Gains)
Real-World Snapshots: Integration in Action
1. The Mid-Sized Regional Health System
A 350-bed system was struggling with a popular direct-to-consumer telehealth platform that was completely disconnected from its EHR. Schedulers were spending over 20% of their day manually reconciling appointments. By implementing a FHIR-based integration for scheduling and registration, they created a unified master schedule for all virtual and in-person visits. Within six months, their no-show rate for telehealth appointments dropped by over 50%, and patient satisfaction with the booking process soared.
2. The Urban Academic Medical Center
An academic center needed to streamline its complex tele-specialty consult workflow. Visiting specialists were unable to easily access patient histories or file their reports back into the leading EHR, causing significant delays. They deployed an integration solution using SMART on FHIR, allowing the specialty platform to launch securely from within the EHR. This gave specialists immediate access to the complete patient chart and allowed them to post their findings directly back into the record. The result was a 15% increase in provider productivity and a significant reduction in the average turnaround time for consult reports.
3. The Rural Health Network
A network of rural clinics relied on telehealth to provide access to care but faced significant billing challenges. Charges from virtual visits were manually transcribed, leading to errors and long delays in reimbursement. They implemented an automated workflow that extracted charge codes from the provider’s finalized telehealth note and sent them directly to the billing system via an HL7 interface. This simple integration slashed their average A/R days for telehealth services by 10 days, dramatically improving cash flow for the critical-access network.
Future-Proofing Your Investment: The Innovation Edge
A well-designed integration strategy does more than solve today’s problems; it builds the foundation for tomorrow’s innovations.
- TEFCA Readiness: The Trusted Exchange Framework and Common Agreement is creating a national “interstate highway” for health data. A modern, FHIR-based integration architecture positions your organization to be a seamless participant in this national network.
- Federated Analytics: You can gain powerful insights from data across multiple systems (e.g., correlating virtual visit trends with population health data) without having to move all the data into a single, monolithic warehouse. This is a more secure and agile approach to analytics.
- AI-Powered Routing & Remote Monitoring: Future AI tools will intelligently route patients to the proper care setting (virtual vs. in-person) based on real-time data. An integrated system is the prerequisite for feeding these algorithms the information they need and for seamlessly connecting data from at-home monitoring devices.
Three Forward-Looking Recommendations:
- Adopt a FHIR-First API Strategy: Mandate that all new digital health tools must have a robust, well-documented FHIR API.
- Design for a Modular Architecture: Avoid monolithic solutions. A modular, microservices-based approach allows you to add or replace components (like a new telehealth platform) without rebuilding your entire ecosystem.
- Prioritize a Central Integration Engine: Invest in a dedicated integration platform rather than relying on brittle, point-to-point connections. This provides centralized governance, security, and scalability.
Conclusion: From Disconnected Tools to a Unified Care Ecosystem
Telehealth integration is the essential, strategic work that transforms a collection of digital tools into a cohesive, intelligent, and efficient system of care. By bridging the gap between virtual and in-person experiences, you empower your clinical teams, delight your patients, and unlock the data-driven insights needed to thrive in the new era of hybrid healthcare.
The journey from a fragmented present to an integrated future requires a clear vision and an experienced technical partner.
Ready to move from fragmented workflows to a unified care ecosystem? Schedule a complimentary, no-obligation architecture consultation with a Logicon’s integration specialist today.