Subscribe to our newsletter
Abstract
Every hospital upgrade is billed as “transformational,” yet the Monday after go-live often delivers duplicate orders, missing notes, and a command center that feels more like an emergency bunker. After two decades inside those war rooms, I’ve learned that success rarely hinges on the shiny new EHR. It depends on the integration patterns that sit between that EHR and everything else. The seven patterns below have weathered Cerner-to-Epic leaps, MEDITECH sunsets, and more patch weekends than I care to count. Embed them now, and your next upgrade will feel routine instead of ruinous.
The Pain Behind the Progress
At 07:58 a.m. on 6 January, cardiologist Dr Langston opened what should have been a simple discharge summary. Instead, she found three nearly identical documents, none of which displayed the troponin trends she needed to clear her patient. The new system had gone live forty-eight hours earlier; however, the integration scripts that were supposed to deduplicate HL7 messages didn’t survive the vendor patch. Pharmacy queues ballooned, transport teams circled for bed status updates, and the CIO—normally a calm presence—started triaging interface tickets like trauma cases.
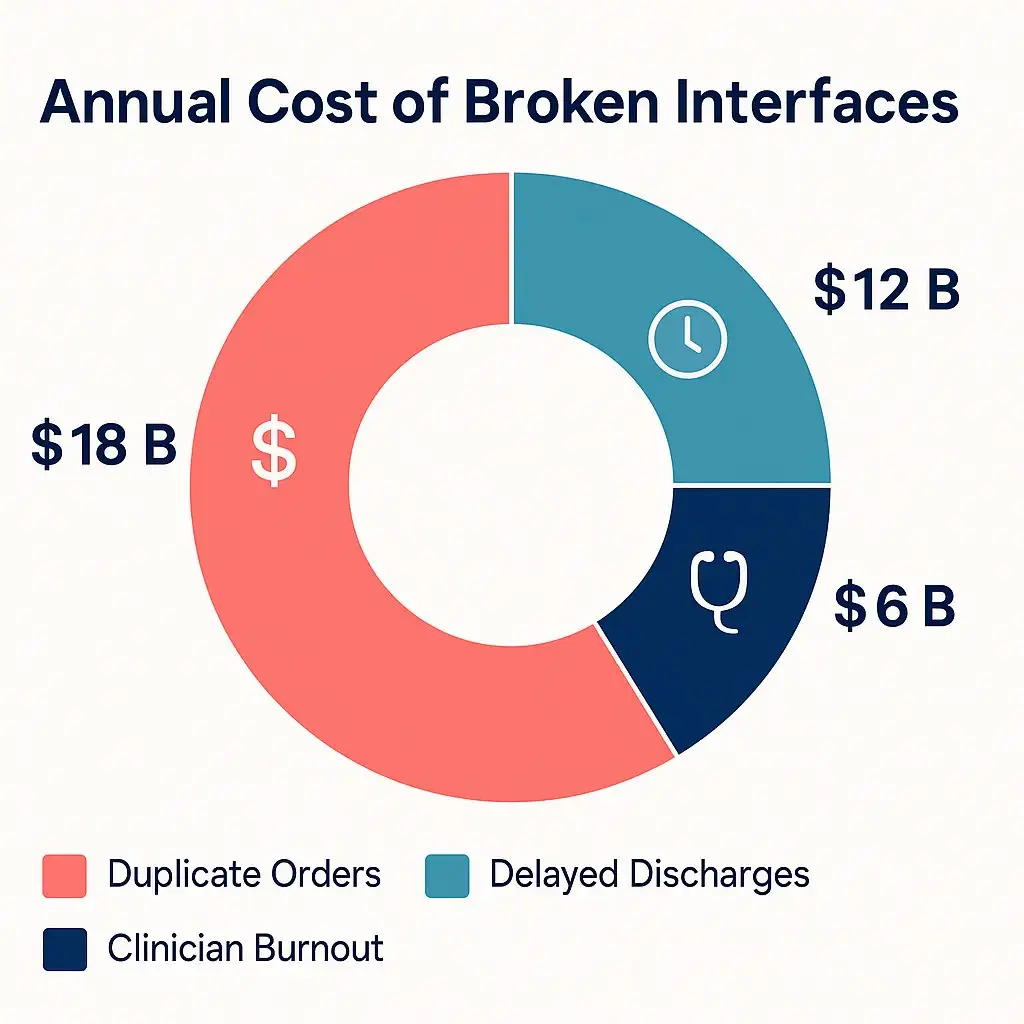
Episodes like this echo across health systems worldwide. Analysts estimate the annual cost of poor interoperability in the tens of billions of dollars. Still, those ledger lines don’t capture the bedside confusion or the extra day a patient spends in a noisy ward waiting for the correct data to appear. The root cause is simple: most hospital interfaces were built for a world that never changes. Software, unfortunately, never stops.
So how do the hospitals that don’t implode manage it? They invest in patterns that assume disruption, isolate risk, and keep clinical workflows breathing even when the digital heart is on the operating table.
7 Patterns That Refuse to Break
1. API-First Architecture – Speak FHIR, Not Folklore
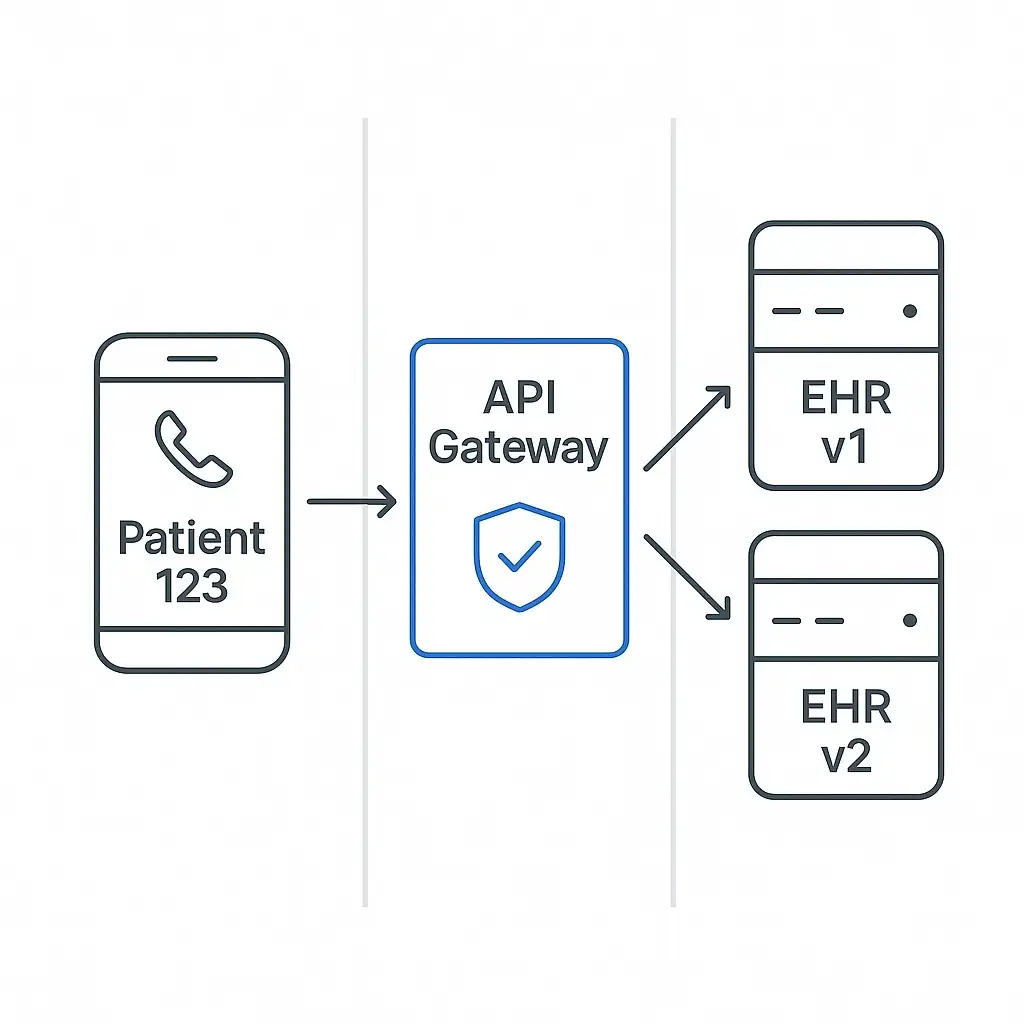
When every application publishes a well-documented REST endpoint—think “Patient 123 Observations”—integration stops being a custom craft and becomes a repeatable science.
Hallmarks of the Pattern
- REST calls secured with OAuth 2.0, throttled at an API gateway.
- Payloads expressed as FHIR resources, so “allergies” mean the same thing everywhere.
- Central analytics showing which consumers are noisy, slow, or misbehaving.
- Strict version tags (v1, v2) that let old apps keep working while new ones evolve.
Why It Survives Upgrades
Swap the EHR, and you only redirect one gateway connection. Downstream apps still call the duplicate URLs, blissfully unaware that the data now comes from Epic instead of Cerner. During a recent Midwest migration, the integration team reduced interface test time from six weeks to eleven days using this exact setup.
2. Event-Driven Pub/Sub–Systems That Announce, Not Poll
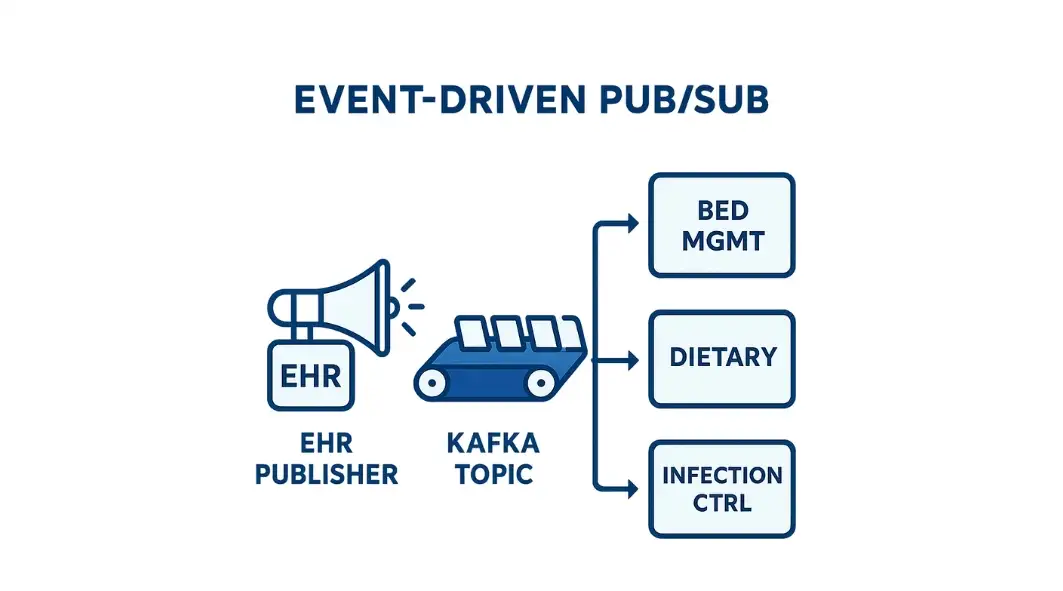
Imagine your EHR broadcasting ‘PatientAdmitted‘ the instant the wristband is printed. Bed management, dietary, and infection control all subscribe, update, and move on—no nightly batch, no brittle query.
Core Mechanics
- Message broker (Kafka, RabbitMQ, or cloud equivalent) stores an immutable stream of events.
- Publishers fire and forget; subscribers process asynchronously.
- Replay capability for audits or backfills.
- Horizontal scaling that eats surge volumes for breakfast.
Upgrade Super-Power
Because publishers and subscribers never meet, replacing the publisher (your new EHR) is like swapping a trumpet in a jazz band—the tune continues. One 700-bed academic center logged forty-seven seconds of Downtime during a full vendor change because the broker buffered every event until the cut-over flag lifted.
3. Integration Hub (Modern ESB or iPaaS) – The Air-Traffic Tower
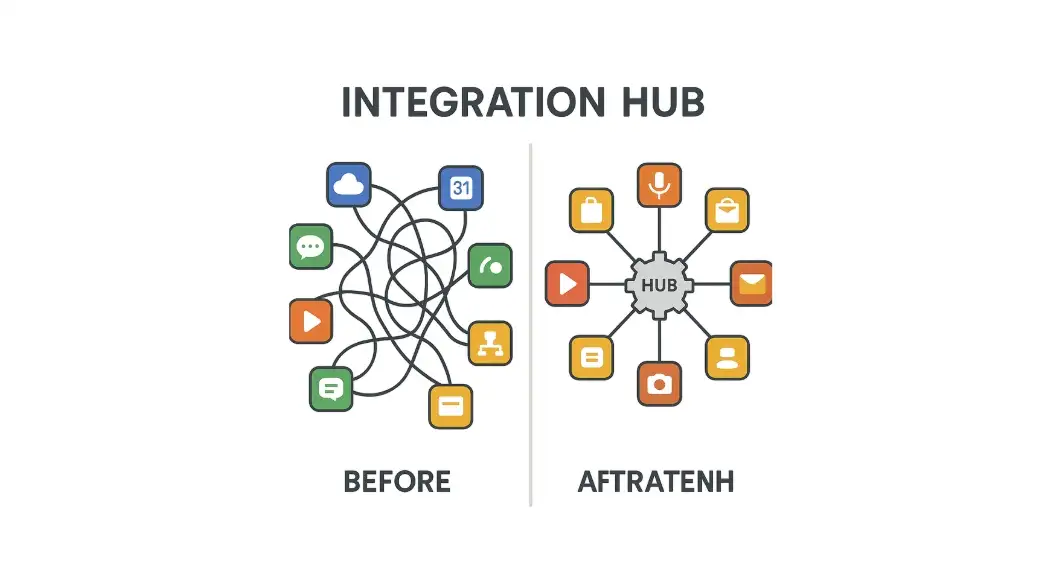
Some hospitals still require classic HL7 v2, while others utilize mobile apps based on JSON. A hub mediates between them, translating dialects so no one crashes on the runway.
What It Looks Like
- Adapters on the perimeter convert protocols to an internal Canonical Model.
- Orchestration engine sequences multi-step workflows—ADT to Bed Board to Pager.
- Central console shows errors and the message that caused them.
- Reusable maps so “pharmacy lookup” isn’t reinvented fourteen times.
Upgrade Advantage
Only the adapter communicating with the EHR changes; fifty ancillary systems remain untouched. A five-facility network avoided 8,000 engineering hours by keeping its hub logic intact during a phased MEDITECH retirement.
4. Logical Data Warehouse – One Truth, Many Sources
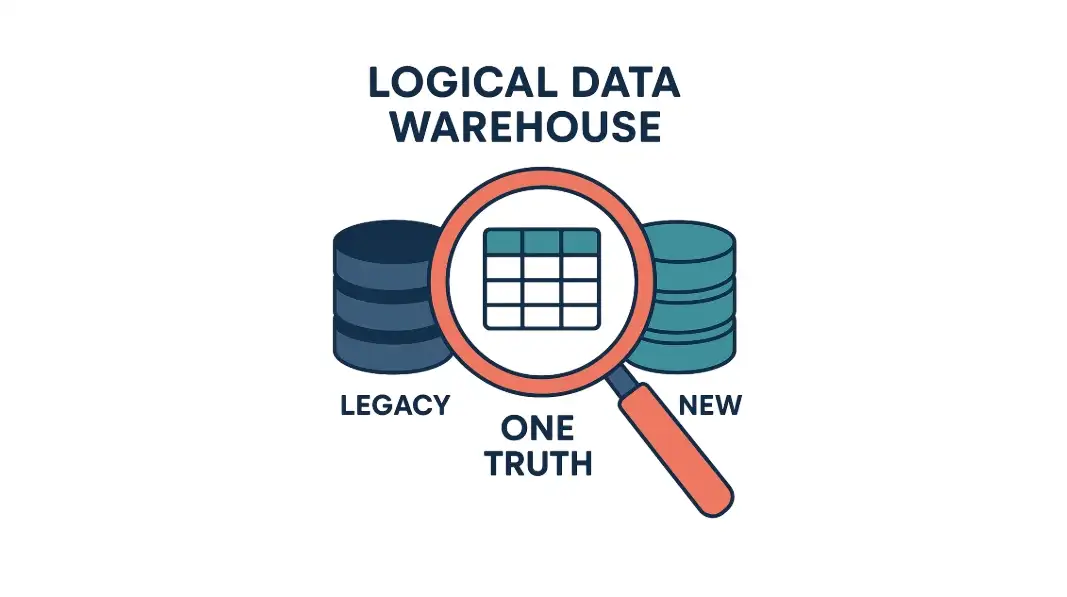
Analytics can’t wait a year for complete data migration. A virtualization layer integrates legacy and new databases into a single, live, and queryable whole.
Signature Traits
- Data stays where it is; the layer federates queries in real-time.
- Role-based security passes through to every source.
- Column names mapped once, reused by every dashboard.
- Hot-swap capability: retire the old source, point views to the new, users never notice.
Why It Shines Mid-Upgrade
Quality measures, sepsis bundles, and payer reports continue without blackout. One IDN’s BI team maintained 427 dashboards for eighteen months while their core clinical data transitioned platforms beneath the surface.
5. Microservices in Containers – Small Pieces Loosely Joined
Monoliths magnify risk: change one line, deploy a house of cards. Microservices isolate that risk to a Lego brick you can swap at will.
Key Ingredients
- Each service owns its code, database table, and runtime container.
- CI/CD pipeline pushes daily without halting the neighbors.
- Sidecar proxies manage logging, security, and traffic shaping.
- Language freedom—Rust for speed, Python for inference, Java for compliance.
Resilience Pay-Off
Only services that communicate with the EHR when care changes. During the upgrade, the scheduling microservice was rewired to the new API; telehealth, billing, and patient feedback services remained untouched.
6. Immutable Data Ledger – Trust That Outlives the Vendor
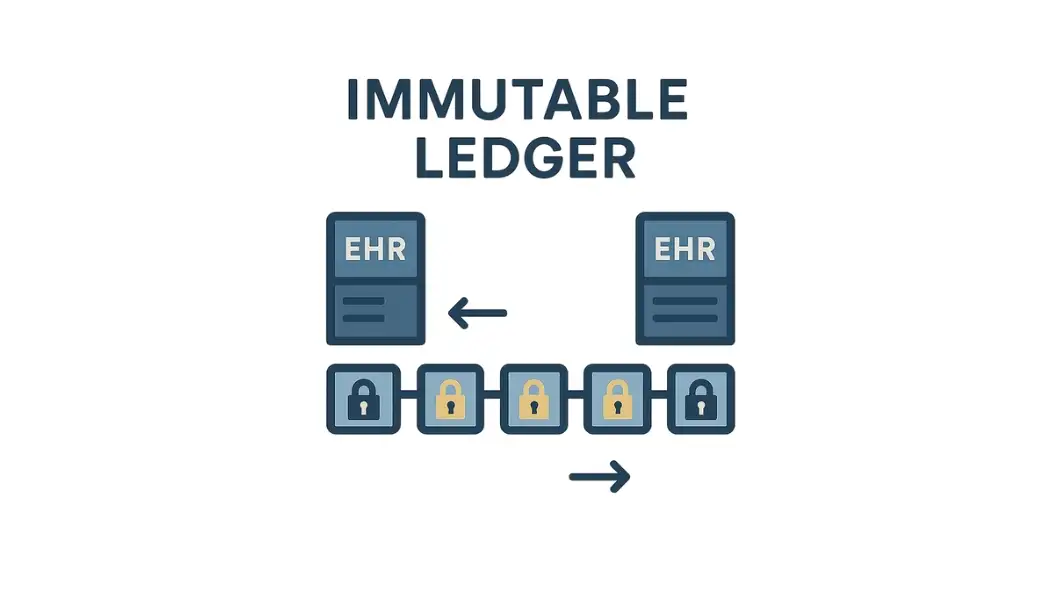
For patient consent, advance directives, or chain-of-custody logs, “maybe” is unacceptable. A distributed ledger writes once and argues never.
How It Works
- Permissioned blockchain nodes across partner hospitals.
- Cryptographic hashes verify every update.
- Smart contracts alert when consent is revoked, or the device is recalled.
- Bulk data stored off-chain; ledger holds fingerprints.
Staying Power
Because the ledger is vendor-neutral, both old and new EHRs tap the same truth. In a regional pilot, surgeons checked implant recalls on the ledger via a tablet while the primary EHR rebooted—no gap, no guesswork.
7. Edge Computing for IoMT – Intelligence at the Bedside
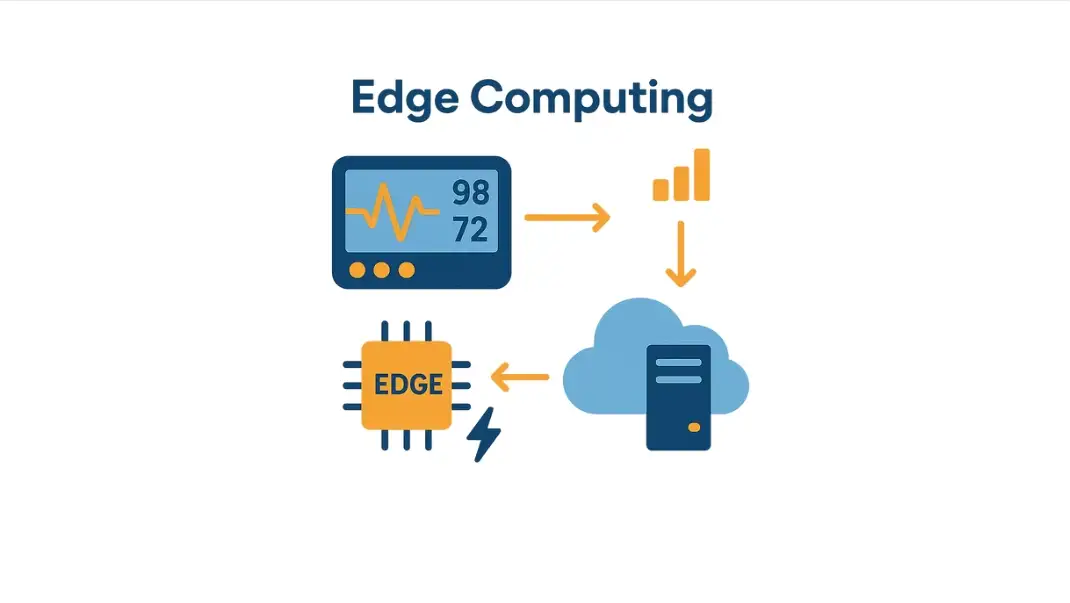
An ICU monitor spits 86,400 heart rate points per patient per day. Ship that raw stream to the core, and you drown. Process at the edge and forward only what matters.
Deployment Pattern
- Gateway appliance or local microcontroller summarises or flags anomalies.
- Temporary buffer saves data during network blips.
- Updates delivered over the air without wheeling a cart.
- AI models tuned to each device, each ward.
During Upgrade
Even if the network is segmented for cut-over, edge devices continue to monitor, buffer, and alert. Once the green light is returned, summaries are flushed to the EHR, backfilling the record without requiring human intervention.
Five-Step Implementation Playbook
- Governance Before Gadgets
Form a cross-disciplinary council—IT, nursing, finance, and security. Empower it to block any project that ignores FHIR R4 or your versioning policy.
- Write the Versioning Constitution
Semantic versions, two active majors in prod, six-month deprecation clock, automated contract tests in CI. Print it, laminate it, and pin it in the war room.
- Pilot Where the Pain Is
Select a brittle process—labs to EMR, discharge medications to pharmacy. Rebuild it with pub/sub plus FHIR. Show a 70 % drop in duplicate messages; use that victory to unlock the budget for the rest.
- Observe Everything
Deploy distributed tracing so one patient ID reveals its journey from wristband scan to KPI dashboard. Alert on error budgets, not just uptime.
- Migrate in Rolling Quarters
Catalogue every interface: retain, refactor, retire. Tackle the top 20 % of pain first, then let sunset dates drive the rest. By year two, point-to-point spaghetti should be museum artifacts.
Executive Dashboard – Metrics That Matter
| KPI | Target | What Success Feels Like |
| Integration TCO | ↓ 20 % in 24 months | Fewer custom feeds, less midnight firefighting. |
| App On-Boarding Time | < 30 days | Innovation Ivy smiles when pilots launch on schedule. |
| Upgrade Downtime | < 45 minutes | Clinicians barely notice the switch-over. |
| Duplicate Orders | ↓ 75 % | Lab and radiology queues unclog, patient flow accelerates. |
| MTTR Critical Feed | < 15 minutes | Command centre resolves issues before wards call. |
| After-Hours Pager Volume | ↓ 50 % | Interface team burnout plummets, retention climbs. |
Quick Win Checklist
- Inventory interfaces and tag each item as red, amber, or green.
- Mandate FHIR for the next mobile app project.
- Spin up a proof-of-concept Kafka topic for ADT events.
- Publish the versioning policy on Confluence today.
Compliance & Security Spotlight
- Encrypt Everything – TLS in motion, AES-256 at rest, including broker disks and container volumes.
- Zero-Trust Tokens – Least-privilege OAuth scopes; break-glass accounts time-boxed and audited.
- Immutable Logs – Message brokers, API gateways, and ledgers keep tamper-evident trails that satisfy HIPAA disclosure audits without added tooling.
Peering Over the Horizon
Change will accelerate, not slow. AI services are already mapping exotic lab codes to standard vocabularies in real-time. Edge devices are now running federated learning models that adapt to each ward’s patient mix overnight. Distributed identity frameworks promise a future where patients, rather than institutions, decide who can access their data.
None of those advances will land safely on yesterday’s point-to-point wiring. By adopting the seven patterns above, you lay tracks that flex with every turn. The next vendor swap, regulatory push, or pandemic surge becomes an engineering exercise—not a crisis call at dawn.
Ready to de-risk your next Epic upgrade? Schedule a strategy session with Logicon’s integration architects.