Subscribe to our newsletter
The electronic health record (EHR), once hailed as a revolutionary tool, is now a primary driver of physician burnout and a drag on hospital margins. The crisis is undeniable, but the solution is hiding in plain sight. Strategic EHR optimization is no longer a “nice-to-have” IT project; it is a critical business imperative. By moving beyond basic maintenance to a proactive, data-driven approach, health systems can transform the EHR from a source of friction into a force for efficiency. This guide details five proven tactics—from physician-led workflow redesign and intelligent customization to advanced training and robust governance. These strategies directly address the usability gaps that frustrate clinicians, giving them back valuable time, protecting the bottom line, and future-proofing their most critical technology investment.
The Staggering Cost of Physician Burnout
The physician burnout crisis has reached epidemic levels, and its impact is measured in both human and financial terms. Today, an alarming 63% of physicians report symptoms of burnout, a figure that has climbed steadily in recent years. This isn’t just a morale issue; it’s a multi-billion-dollar problem. The U.S. healthcare system loses an estimated $4.6 billion annually due to the direct costs of physician turnover and reduced clinical hours. With the cost to replace a single physician ranging from half a million to over a million dollars, no health system can afford to ignore the root causes.
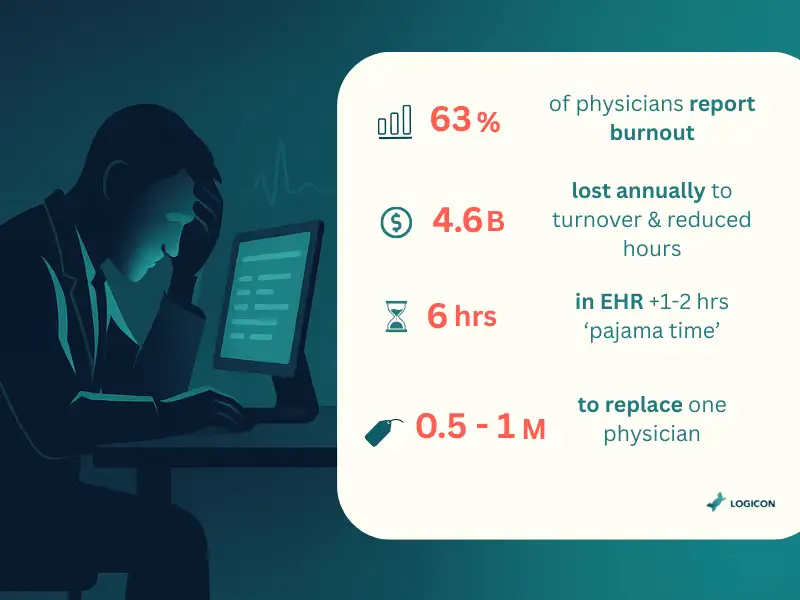
A significant portion of that burnout can be traced directly to the EHR. Clinicians now spend an average of nearly six hours on the EHR during their clinic day, plus another one to two hours of “pajama time” on documentation after hours. This administrative overload, fueled by clunky interfaces and inefficient workflows, is a direct threat to both patient care and financial stability. The path to a healthier organization runs directly through a smarter, more usable EHR.
Tactic 1: Physician-Led EHR Workflow Redesign
The most effective optimization efforts don’t start in the IT department; they begin at the elbow of the clinician. By observing and redesigning the most common workflows, health systems can eliminate thousands of unnecessary clicks and hours of wasted time.
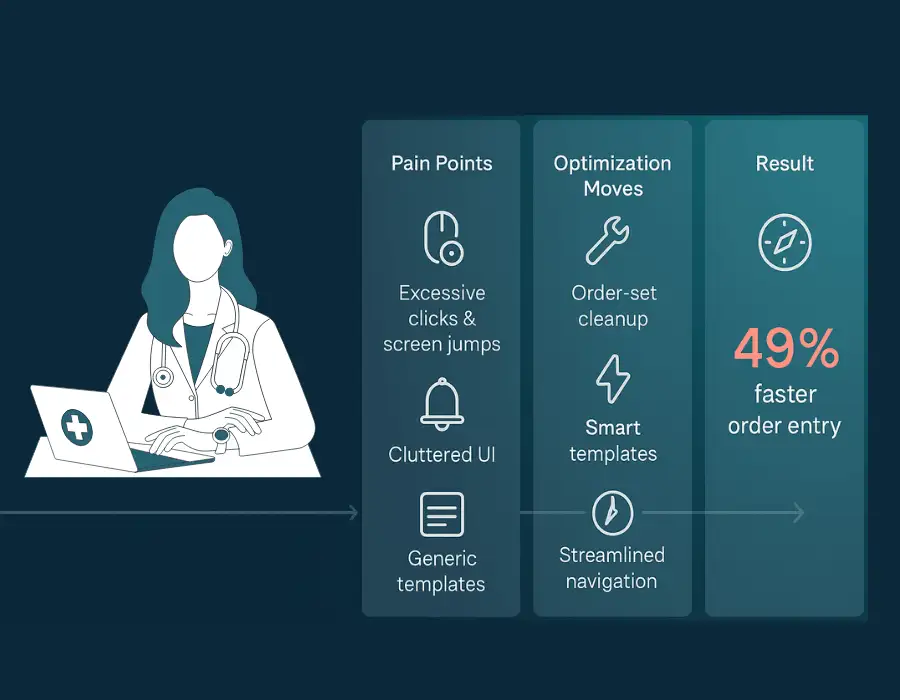
The Pain Points:
- Excessive clicks and screen jumps are required to perform simple tasks like placing an order.
- Alert fatigue from an overwhelming number of irrelevant pop-ups.
- Cluttered user interfaces that hide critical information.
- Poorly designed templates that don’t match specialty-specific needs.
Optimization Moves:
- Order Set Refinement: Collaborating with physicians to clean up and streamline Computerized Provider Order Entry (CPOE) sets for the 20 most common diagnoses.
- Smart Template Development: Building specialty-specific note templates and SmartPhrases that automatically pull in relevant data.
- Navigation Streamlining: Redesigning preference lists and dashboards to surface the most frequently used functions, reducing search time.
Implementation Essentials:
This requires a hands-on approach, including time-motion studies to quantify clicks and time-per-task. Prototyping and A/B testing new designs with a core group of physician champions ensures the final product solves the problem.
KPI Snapshot & Mini-Case:
- Metrics: Clicks-per-order, time-to-complete-note, user-satisfaction scores.
- Vignette: A leading academic medical center focused on redesigning its medication ordering process. By engaging physicians to rebuild their most-used order sets and preference lists, they cut the time required to place complex orders by 49%. This not only saved time but also reduced potential errors, a win for both the operations director and the chief information officer.
Tactic 2: Advanced Training & Personalization
The initial, one-size-fits-all EHR training that physicians receive during onboarding is rarely sufficient. Continuous, personalized education is one of the highest-ROI investments a hospital can make.
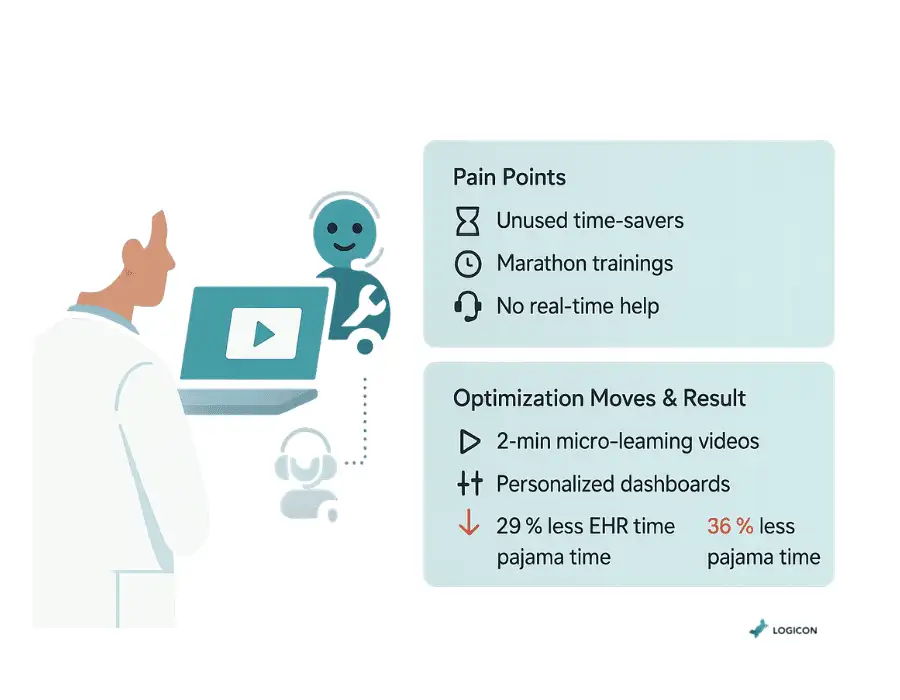
The Pain Points:
- Physicians are unaware of time-saving features and personalization options.
- Training is delivered in long, inconvenient sessions that are quickly forgotten.
- Lack of at-the-elbow support to solve problems in real-time.
Optimization Moves:
- Micro-learning Modules: Replace lengthy classroom sessions with a library of short (2-3 minute), on-demand videos that teach specific skills, accessible directly from the EHR.
- Personalization Workshops: Host dedicated sessions where IT trainers work with small groups of physicians to customize their dashboards, templates, and preference lists.
- At-the-Elbow Support: Deploy “EHR rover” support staff who can provide immediate, in-clinic assistance to physicians, resolving issues on the spot.
Implementation Essentials:
Success requires a shift from a “training event” mindset to a “continuous learning” culture. This must be supported by leadership and integrated into the clinical day.
KPI Snapshot & Mini-Case:
- Metrics: Time spent in the EHR, after-hours documentation time, and help-desk ticket volume.
- Vignette: A Colorado-based health system launched a targeted personalization program for its primary care physicians. After just two one-hour sessions and follow-up at-the-elbow support, the physician group saw a 29% reduction in their average time spent in the EHR and a 36% drop in after-hours “pajama time.”
Tactic 3: Team-Based Documentation & Task Distribution
Requiring physicians, the most highly trained and expensive members of the care team, to perform extensive clerical work is a profound operational failure. Empowering the entire team to contribute to documentation is essential.
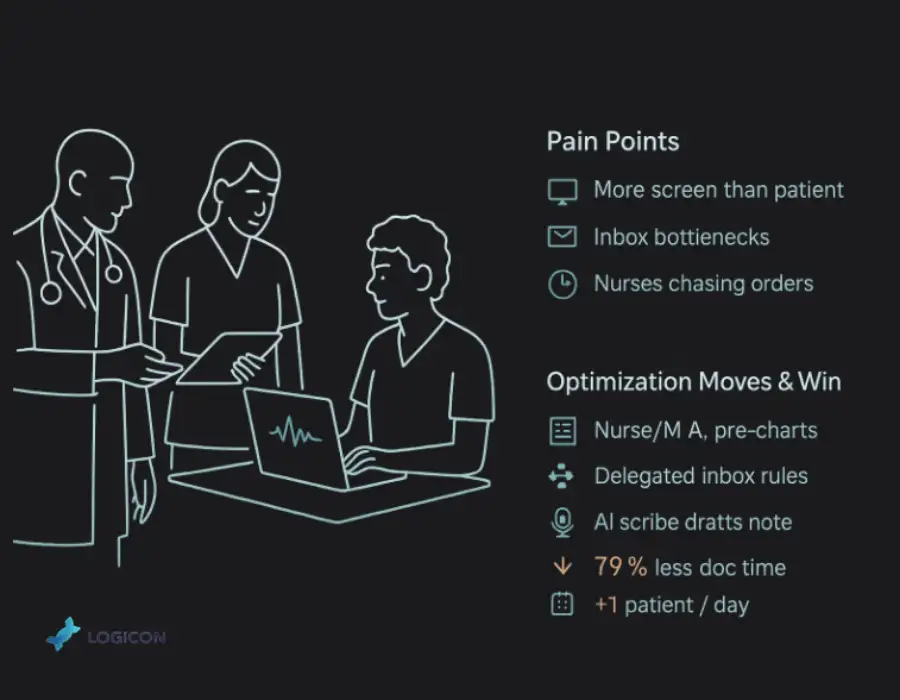
The Pain Points:
- Physicians spend more time on the computer than with the patient.
- The physician’s inbox becomes a bottleneck for routine patient communication and results management.
- Valuable nursing time is wasted tracking down physicians for simple orders.
Optimization Moves:
- Team Documentation: Implementing workflows where nurses or medical assistants can “pend” orders, tee up note templates, and document parts of the patient history for the physician to review and sign.
- Inbox Delegation: Creating clear protocols that allow nurses and MAs to manage routine inbox messages (e.g., prescription refills, normal lab results) on behalf of the physician.
- AI Scribe & Ambient Intelligence: Deploying AI-powered tools that listen to the patient-provider conversation and automatically draft the clinical note.
Implementation Essentials:
This requires strong governance to ensure all delegated tasks fall within the staff member’s scope of practice. For the CIO, ensuring these workflows are secure and auditable is critical. For the operations director, clear communication about the new roles and responsibilities is vital.
KPI Snapshot & Mini-Case:
- Metrics: Time spent on documentation, inbox message volume, patient face-time.
- Vignette: A large multi-specialty clinic implemented a team-based model using scribes. The program slashed physician documentation time by an incredible 79%. This allowed the clinic to add one additional patient slot per physician per day, directly improving both revenue and patient access.
Tactic 4: Intelligent Customization & Third-Party Apps
The core EHR is a platform, not a complete solution. The safest and fastest way to enhance its capabilities is by integrating best-in-class third-party applications through a secure, well-governed process.
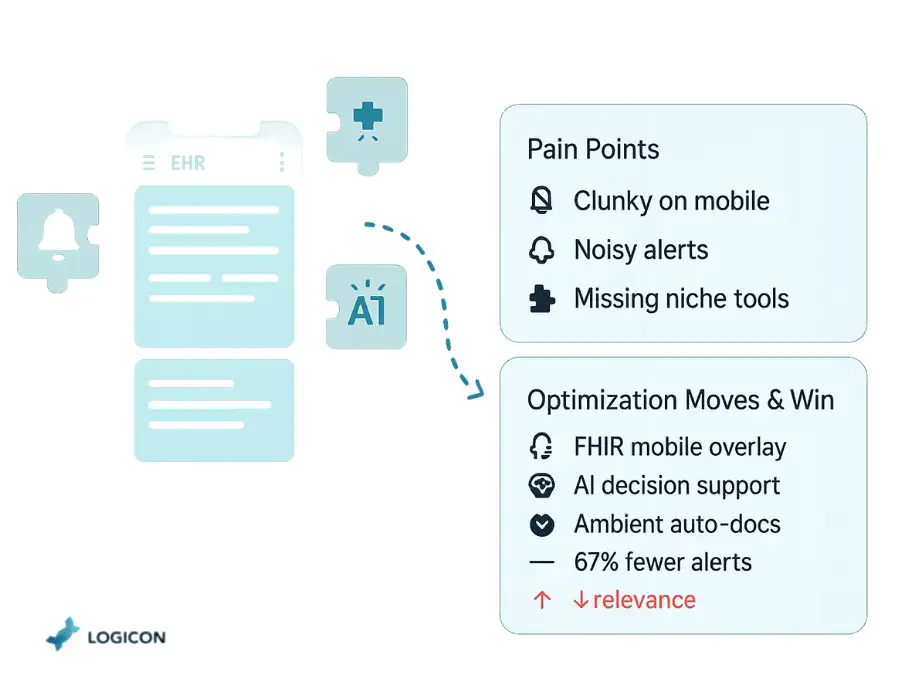
The Pain Points:
- The native EHR user interface is clunky, especially on mobile devices.
- The built-in clinical decision support (CDS) is overly simplistic or generates too many irrelevant alerts.
- The enterprise system does not adequately support niche specialty workflows.
Optimization Moves:
- Mobile Overlays: Implement secure, FHIR-based mobile apps that provide a simplified, intuitive interface for everyday tasks like rounding, charge capture, and secure messaging.
- Intelligent CDS: Integrate advanced decision support tools that use AI to provide more relevant, evidence-based alerts at the point of care.
- Ambient Intelligence: Deploy AI tools that automatically handle documentation, as mentioned in Tactic 3.
Implementation Essentials:
This is where a mature integration strategy becomes a competitive advantage. A CIO must establish a governance framework for evaluating and approving third-party apps, with a focus on security, interoperability, and clinical value. Working with an enterprise integration partner like Logicon ensures these apps are connected via modern, secure Fast Healthcare Interoperability Resources (FHIR) APIs, not brittle, legacy interfaces.
KPI Snapshot & Mini-Case:
- Metrics: Alert acceptance rate, clicks-per-task, time spent on mobile devices vs. workstations.
- Vignette: An inpatient pharmacy team was struggling with alert fatigue from the EHR’s native medication warning system. They integrated a specialized third-party CDS tool that analyzed patient data more intelligently. The new system reduced medication-related alerts by 67% while increasing the clinical relevance of the remaining alerts, improving both safety and workflow.
Tactic 5: Data-Driven Optimization & Governance
You cannot improve what you do not measure. The most mature health systems treat EHR optimization as a continuous, data-driven program, not a series of disconnected projects.

The Pain Points:
- Optimization efforts are based on anecdotal complaints from the loudest voices.
- No objective way to measure whether changes are improving workflows.
- IT and clinical teams operate in silos, leading to conflicting priorities.
Optimization Moves:
- EHR Utilization Analytics: Deploy tools that passively analyze usage patterns to pinpoint exactly where clinicians are losing time—which screens, which buttons, which workflows.
- Establish a Governance Committee: Create a multidisciplinary optimization council with representatives from IT, operations, nursing, and key physician specialties to review the data and prioritize projects.
- Implement Quarterly Improvement Cycles: Use the data to identify, implement, and measure the impact of 2-3 high-priority optimizations every 90 days.
Implementation Essentials:
This requires a cultural commitment to transparency and continuous improvement. The data must be used for process improvement, not to punish individuals.
KPI Snapshot & Mini-Case:
- Metrics: After-hours EHR usage, specialty-specific efficiency benchmarks, and burnout scores.
- Vignette: The Cleveland Clinic used utilization data to drive its optimization program. By identifying and fixing workflow inefficiencies revealed by the data, they were able to reduce after-hours EHR work by 44% across their physician enterprise, a massive win for work-life balance and retention.
An Achievable Implementation Roadmap
A successful EHR optimization program is a marathon, not a sprint. A phased approach ensures early wins and sustainable progress.
- Readiness & Data Audit: Assess your current state. Analyze EHR utilization data to identify the top 5-10 sources of clinical friction.
- Establish Governance: Form your multidisciplinary optimization committee to ensure alignment between IT, operations, and clinical leadership.
- Prioritize Quick Wins: Use an impact/effort matrix to select one to two pilot projects. An ideal pilot is high-impact and low-complexity, such as refining ED order sets or deploying a mobile charge capture app.
- Execute Pilot & Measure: Launch the pilot in a contained environment. Meticulously track the baseline and post-implementation KPIs.
- Build the Business Case: Use the pilot’s success and ROI data to secure executive support for a broader, specialty-by-specialty rollout.
- Scale, Measure, Repeat: Expand the program across the enterprise while establishing a continuous feedback loop using utilization data to inform the next round of priorities.
Building the Business Case for the Board
For the CIO, framing optimization as a strategic investment in margin protection is key.
Breakeven Point (in months) = Program Cost / (Cost of Physician Turnover Avoided)
A dashboard for the board should focus on a handful of powerful metrics:
- Physician Turnover Rate: The ultimate measure of burnout’s financial impact.
- After-Hours EHR Time: A direct indicator of work-life balance and a leading indicator of burnout risk.
- Clicks-per-Note/Order: A simple, powerful proxy for EHR usability and efficiency.
- Patient Throughput: Show how faster documentation and ordering cycles improve operational flow.
Pitfalls & How to Avoid Them
| Common Pitfall | How to Mitigate It |
| Treating it as a one-off “IT project” | Establish a permanent, multidisciplinary governance committee that meets quarterly. |
| Lack of genuine clinical leadership | Appoint and empower respected physicians and nurse champions for every specialty. |
| Underestimating integration complexity | Partner with an enterprise integration expert to manage the secure connection of third-party apps and data sources. |
| “Check-the-box” training | Invest in modern, personalized, at-the-elbow training and on-demand micro-learning resources. |
| Failing to measure impact | Deploy EHR utilization analytics from day one to baseline performance and prove ROI. |
Future-Proofing Your EHR Investment
The EHR platform of tomorrow will be more intelligent, automated, and open. Preparing for this future starts today.
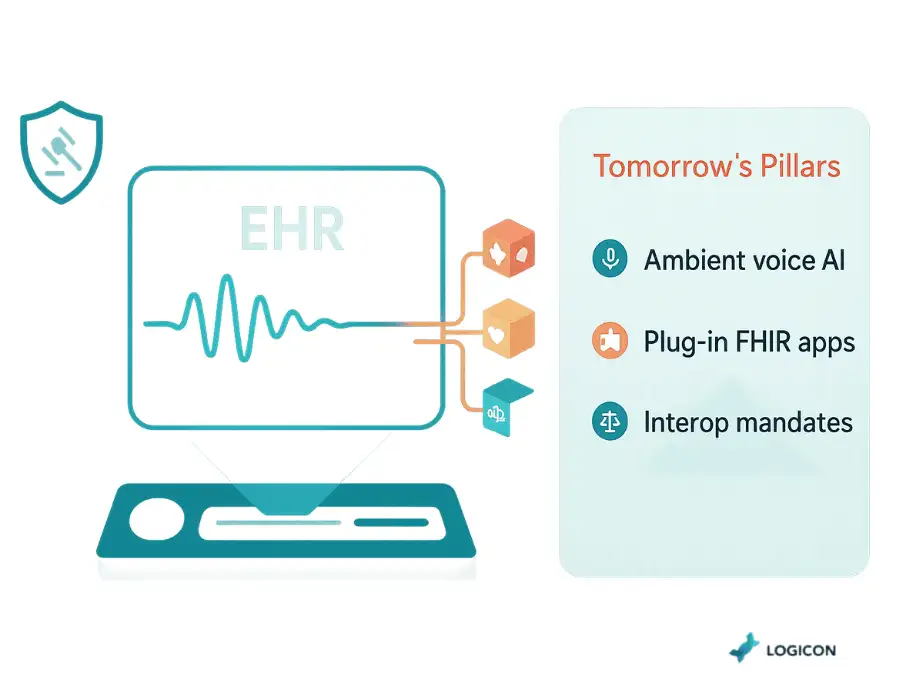
- Ambient AI: Voice-driven, ambient intelligence will become the standard for documentation, making the keyboard and mouse obsolete for clinical notes.
- FHIR-Native Apps: The ecosystem of secure, plug-and-play third-party apps will continue to grow, allowing for rapid innovation on top of the core EHR.
- Regulatory Shifts: Federal rules will continue to demand greater interoperability and data transparency.
Three Recommendations to Prepare:
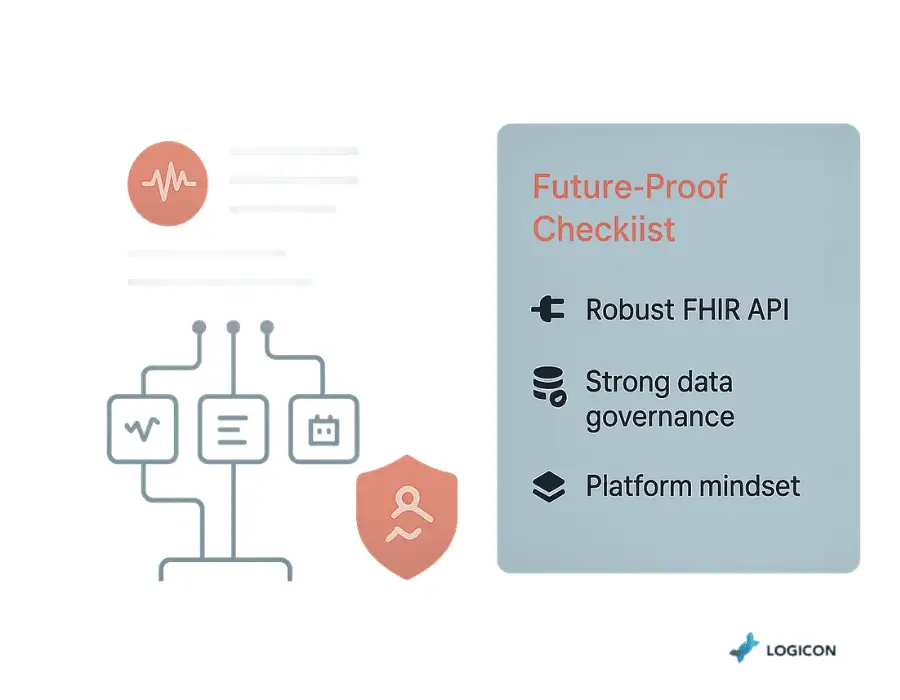
- Build a Robust API Layer: A modern, FHIR-based integration architecture is the most critical prerequisite for future innovation.
- Prioritize Data Governance: Clean, standardized data is the fuel for all future AI and analytics initiatives.
- Think Platform, Not Product: Treat your EHR as a platform upon which you can build and integrate best-in-class tools, rather than a monolithic, closed system.
Conclusion: From Burden to Asset
Your EHR does not have to be a source of frustration and financial drain. With a strategic, clinician-centric, and data-driven approach, it can be transformed into your organization’s most powerful asset for improving efficiency, supporting your care teams, and delivering high-quality patient care. This transformation requires a partner who understands both the technical complexities of enterprise integration and the human realities of the clinical workflow.
Ready to turn your EHR from a liability into a strategic asset? Book a complimentary 30-minute EHR optimization consultation with Logicon’s experts today.